Hearing Loss
Because we live in a hearing world, one of the main goals of our practice is to provide restoration of sound, personalized to your specific hearing needs and concerns. We achieve this through ossiculoplasty, hearing amplification and cochlear implants. Every individual’s hearing needs are unique.
Conductive (mechanical) hearing loss
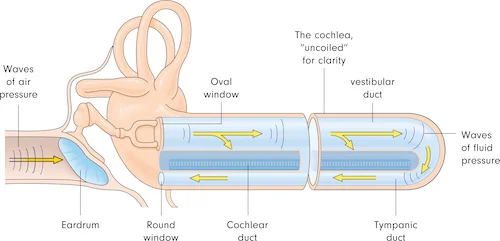
Conductive hearing loss occurs when sound reaching the middle ear is incompletely transmitted to the sensory cells in the cochlea, the organ of hearing. It can be the result of obstruction of the ear canal due to cerumen or masses/lesions of the canal. It can also result from problems of the eardrum, the small bones of hearing behind the eardrum or the middle ear space. This type of hearing loss is often correctable with ossicular chain reconstruction, tympanoplasty or debridement of the ear canal.
Tympanic membrane perforation
Tympanic membrane perforation is the rupture or presence of a hole in the eardrum. The eardrum acts as a barrier between the outer and middle ear and aids in the transmission of sound vibrations to the small bones of hearing. Tympanic membrane perforations can lead to hearing loss. The degree of hearing loss is related to the size and location of the perforation.
Surgical repair is indicated in patients with associated hearing loss, frequent ear infections, or with patient preference. Avid swimmers and divers also benefit from surgery. Dr. Cristobal performs this surgery (tympanoplasty) with a cartilage graft harvested from the tragus.
Ossicular discontinuity
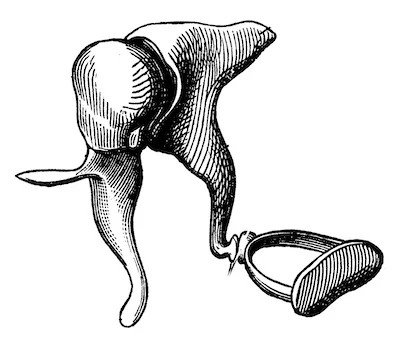
The middle ear space, located in between the eardrum (tympanic membrane) and the organ of hearing (Cochlea), contains three connected bones of hearing called the Malleus (hammer), Incus (anvil), and the Stapes (stirrup) bones.
Sound waves travel through the ear canal and cause the eardrum to vibrate. This in turn vibrates the malleus, which causes the incus to vibrate and then triggers vibration of the stapes bone. The stapes bone then sends vibration into the Cochlea for transmission of sound to the brain. Fixation, malformation, disease, or disruption of any of these 3 bones can result in a conductive hearing loss. Common causes include congenital malformation or fusion of certain bones, erosion from a chronic ear infection or cholesteatoma, or displacement/fracture from head trauma.
Surgical intervention is called an Ossicular Chain Reconstruction or Ossiculoplasty and involves replacing the affected bones of hearing with an artificial bone-like structure called a prosthesis.
Malleus, Incus, Stapes
Otosclerosis
Otosclerosis is an inherited or rarely spontaneous disorder of the bone surrounding the inner ear and the third bone of hearing called the Stapes. It causes decreased vibration of the Stapes and, over months to years, inhibits the ability to properly transmit sound waves into the organ of hearing (the Cochlea). This in turn causes a gradually progressive, conductive hearing loss. Otosclerosis may also affect the bone surrounding the cochlea and cause a sensorineural hearing loss component as well. On a hearing test this shows up as a mixed hearing loss.
Surgical Interventions depend on the severity of hearing loss. If hearing aids do not provide enough amplification, or are not preferred, surgical intervention called a Stapedotomy can be performed. The Stapedotomy is typically performed through the ear canal with the assistance of a laser and titanium prosthesis to replace the Stapes. Correction of the conductive hearing loss is permanent in the large majority of cases.
Cerumen (wax) impaction
Earwax or cerumen is a substance made up of skin cells, hair, and secretions from glands of the outer portion of the ear canal. These components together create a wax like substance which aides in protecting the ear from things like bacteria and fungus. Normally cerumen is expelled from the ear canal in a “conveyor belt” fashion, which occurs as a result of jaw movements. Cerumen buildup can happen to anyone, however it often occurs when there is an interruption of this process. Such situations can include hearing aid use, frequent earplug use, use of q-tips, misshaped ear canals, or with ageing. If cerumen buildup is left un-treated, cerumen impaction can occur causing ear discomfort, infection, and hearing loss. This can be easily removed with the aid of over the counter ear drops for wax, or debridement in our office.
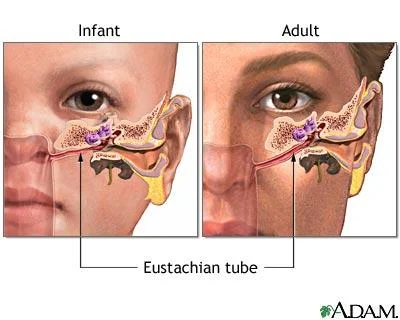
Eustachian tube dysfunction
The Eustachian tube is a tube that sits behind your sinuses and connects the space behind the nose to the middle ear space behind the eardrum. Its job is to protect the middle ear by maintaining an equalized pressure within the middle ear and draining out middle ear fluids. Children commonly have problems with their Eustachian tube as they are often horizontally oriented rather than downward, as in adults. A poorly functioning Eustachian tube keeps it from allowing air into the middle ear, which can cause negative pressure or a buildup of fluid, eventually leading to middle ear effusions and hearing loss.
If medical management with allergy medications and nasal steroids is not enough, surgical intervention includes placement of pressure equalization tubes to prevent infection of the fluid and hearing loss. Some children will need more than one set of tubes during their period of Eustachian tube dysfunction. In adults, pressure equalization tubes can be placed in the office by one of our trained providers.
More recently, new technology has become available that my help with eustachian tube function in the appropriate patients once nasal allergies, and stomach acid reflux have been addressed without success. The eustachian tube dilation procedure entails temporarily dilating the opening of the tube into the nose by briefly inserting a catheter in the nose and inflating a balloon surrounding its tip. Different systems are available. An example of one of them can be seen here:
<iframe width="560" height="315" src="https://www.youtube.com/embed/hJMort6YCI4" title="YouTube video player" frameborder="0" allow="accelerometer; autoplay; clipboard-write; encrypted-media; gyroscope; picture-in-picture" allowfullscreen></iframe>
Sensorineural (nerve) Hearing Loss
Sensorineural hearing loss occurs when there is damage to or dysfunction of the cochlear hair cells or cochlear nerve. This type of hearing loss if often permanent. This can lead to a decrease in perceived sound loudness, with or without deterioration of the clarity of the sound. This may manifest itself as difficulties with speech understanding, which are usually most noticeable in background noise. The causes can range from congenital (present at birth), infectious viral causes, autoimmune disease, or progressive hearing loss related to age, loud sound exposure, or genetics. Oftentimes, no exact cause can be determined.
Such patients frequently lose interest in and avoid social situations, and can suffer from isolation and oftentimes depression. In some instances rapidly progressive hearing loss can result from a treatable medical condition. In such patients, a thorough medical evaluation is indicated and treatment to arrest progression or to improve the hearing may be available. Nevertheless, patients with difficulties communicating can experience an improvement in their quality of life with adequate amplification using correctly fitted hearing aids or cochlear implants.
Sudden Sensorineural Hearing Loss
Sudden Sensorineural hearing loss (SSNHL) is usually a one sided hearing loss which occurs in less than a three day (72hour) period of greater than 30dB in at least 3 consecutive frequencies or pitches, and of inner ear or hearing nerve origin. SSNHL is considered an otologic urgency as delay in diagnosis may decrease the effectiveness of treatment. SSNHL has been estimated to occur in approximately 5 to 20 in 100,000 people per year.
Many times there is no known cause. SSNHL can occur at any age, however commonly occurs in ages 40-50. The causes of SSNHL have been extensively researched, however a lot is still unknown. In some cases, infectious causes, trauma, autoimmune, and vascular or hematologic causes have been identified. Ototoxic medications (Gentamicin) have also contributed to cases of SSNHL. Furthermore, certain disorders of the inner ear such as Menieres’ diseases and Endolymphatic Hydrops can cause periods of SSNHL.
Viral causes of SSNHL are labeled Labyrinthitis. Certain viruses in the Herpes family (HSV1, HSV2, herpes zoster, influenza) cause inflammation and destruction of cochlear and vestibular hair cells leading to sudden hearing loss. Associated symptoms include dizziness, vertigo and ringing in your ears (tinnitus).
Auto-immune causes of hearing loss are very rare, occurring in about 1% of the hearing loss population. This occurs when the body’s immune system attacks its own tissues, specifically within the ear. Allergies and multiple auto-immune illnesses can contribute to this including Sjogren’s syndrome (dry eye syndrome), Rheumatoid Arthritis, systemic lupus erythematosus (SLE), Bechet’s Disease, Wegener’s granulomatosis, Ankylosing Spondylitis, Scleroderma, Cogan’s disease, and ulcerative colitis. Immunological blood tests may help confirm this diagnosis but are not always definitive.
Endolymphatic hydrops is a spectrum disorder of fluctuations in the potassium and sodium containing endolymphatic fluid within the inner ear structures. In some people, cochlear hydrops causes sudden drops in hearing, while more severe endolymphatic hydrops (Meniere’s Disease) causes both drops in hearing and vertigo spells. Often times these episodes of hearing loss are characterized by fluctuations in hearing with an overall decline in hearing over time. The course of hearing decline progresses differently for each individual. There are special medications used for Meniere’s disease listed in the vertigo section of this site.
Medical treatment includes routine monitoring of hearing loss and, if not contraindicated, treatment with corticosteroids either oral or intratympanic (delivered through the eardrum into the middle ear). Unfortunately corticosteroid treatment will not always result in return of normal hearing. Only about half of patients treated with corticosteroids notice an improvement of their hearing. Recent guidelines suggest a role for hyperbaric oxygen treatment primarily or as a rescue attempt. If a specific auto-immune illness is causing hearing loss, further treatment will be required by a rheumatologist.
Even after proper treatment it is possible that the hearing may recover incompletely, remain the same, or even worsen. In the case that hearing remains the same or worsens, hearing interventions may be indicated such as the use of conventional CROS, BiCROS hearing aids, bone anchored hearing aid (BAHA), or cochlear implants.
Surgical interventions after medical treatment fails and hearing aids are not able to amplify to the degree needed, often includes cochlear implantation in those who have bilateral hearing loss severe enough to qualify.
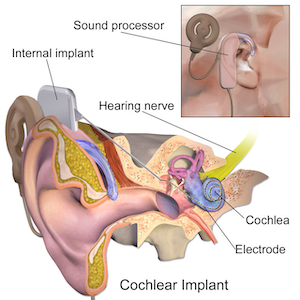
A cochlear implant is a hearing implant that is placed in the cochlea of the inner ear. Cochlear implants directly stimulate the nerve of hearing through an electrode array, thus bypassing the ear canal, eardrum, middle and inner ear. The inner piece is implanted surgically underneath the scalp and into the skull bone behind the ear, while a hearing aid-type outer piece is worn either over the ear, clipped to the clothing, or on an armband. This implant is used for patients who have severe to profound hearing loss in both ears and difficulty understanding speech.
During the surgical procedure, patients may lose any residual hearing that they had prior to surgery, and thus the device is recommended only to those who have little meaningful hearing despite the use of hearing aids. It is the standard of care when hearing aids are not enough, and selected patients typically perform better with cochlear implantation than they do with the hearing aids. However, there are some limitations. Patients that are born deaf perform best when implanted early in life, and typically surgery is scheduled after their first birthday when timely identification and evaluation has been done. There is no upper age limit for implantation so long as the patient is healthy enough to undergo surgery and is motivated to use the device. In a contemporary setting, cochlear implantation is the standard of care for poor speech understanding performance with appropriately fitted hearing aids. The surgical procedure is safe for patients without anesthesia risks, and both the device and surgery are covered by insurance almost universally.
Attributed: Blausen.com staff (2014).
To learn more about the different manufacturers of cochlear implants click below.
As more is discovered about SSNHL, diagnostic testing and treatments may continue to change.
Congenital Hearing Loss
Congenital hearing loss simply means hearing loss was present at birth. It can be caused from genetic disorders (hereditary) or from problems occurring during pregancy or birth.
Nongenetic factors could include:
Maternal infections such as Toxomoplasmosis, Rubella, Cytomegalovirus, and Herpes simplex virus (TORCH)
Maternal consumption of toxins, certain drugs, or alcohol during pregnancy
Maternal Toxemia
Gestational Diabetes
Anoxia (Lack of oxygen) in utero
Birth injuries
Prematurity
Low birth weight
Jaundice or hyperbilirubinemia
Genetic Factors are more commonly the cause of congenital hearing loss. Syndromes associated with hearing loss include:
Down Syndrome
Waardenburg Syndrome
Usher syndrome
Treacher Collins syndrome
Crouzon syndrome
Alport syndrome
Many of the causes of congenital hearing loss, also involve problems with other systems of the body. For this reason, when congenital hearing loss is suspected, in many cases the patient will receive an evaluation by a genetics specialist and ophthalmologist and will also need imaging of the kidneys and the brain.
Regardless of the cause of hearing loss, it is required that children are diagnosed with hearing loss by 6 months of age and are treated within the 1st year of life. To ensure this, in the United States, hearing screening is done just after birth. If a baby does not pass the hearing screen, they are immediately sent for further evaluation. Hearing plays a crucial part in normal growth and development and if present can cause speech delay as well as language and social problems. So if hearing loss is suspected it is important to seek care as soon as possible.
Treatment for congenital hearing loss can vary depending on the type and severity of hearing loss experienced. This could include hearing aids, a bone anchored hearing aid (BAHA), or implantation with a cochlear implant, as discussed above. Treatment will require a collaborative approach with routine monitoring of hearing, frequent adjustments of hearing device, and speech therapy.
Age-related Hearing Loss (Presbycusis)
Presbycusis is a form of hearing loss associated with aging. It is a progressive and symmetrical bilateral sensorineural hearing loss due to a gradual loss of sensory hair cells within the organ of hearing (cochlea). Unfortunately the hair cells do not regenerate and once lost, hearing loss is permanent. Commonly, the loss happens so gradually it is not the patient that recognizes hearing loss, but the family. Family members begin to notice they have to constantly repeat themselves in order for the patient to hear what they are saying. With time, patients may begin to notice they have difficulty with talking on the telephone and have to turn the television volume up very high in order to hear.
Age related hearing loss is generally treated with traditional hearing aid amplification.
Noise Induced Hearing Loss (NIHL)
Noise induced hearing loss is simply hearing loss caused by exaggerated exposure to sound. This relies on two factors, how loud a sound is, measured in decibels (dB) and the extent of time exposed to the sound. Either or both of these two factors in excess can cause damage to sensory hair cells in the inner ear. The hair cells work to convert sound into electrical signals sent to the brain. Unfortunately the damage to these cells is irreversible. Damage can be caused by a one-time exposure to intense sound such as a blast or gunfire, or from extended daily exposure. Typically, this hearing loss increases gradually with exposure over time. Noise induced hearing loss is the only form of hearing loss that is 100% preventable. The use of ear-plugs and noise canceling ear muffs can help protect your ears during loud sound exposure.
Treatment of NIHL includes routine monitoring with hearing tests and use of hearing aids. Wearing ear protection to prevent further damage is of paramount importance.
Central Auditory Processing Disorder
Central Auditory Processing Disorder (CAPD) is a term used to describe a processing disorder that may vary based on the perspective of the professional describing the problem. Symptoms include difficulty localizing sound, difficulty understanding spoken language in competing messages or background noise, taking longer to respond in oral communication situations, inconsistent or inappropriate responding, difficulty comprehending and following rapid speech or complex auditory directions. Patients with CAPD can have conductive, sensorineural, and mixed hearing loss, as well as auditory neuropathy. Appropriate audiological, as well as speech and behavioral tests should be administered by an experienced professional.
Treatment includes using a team approach to assess all needs. Depending on the needs of the individual, team members may include an audiologist, speech language pathologist, a teacher, parents, and a counselor.