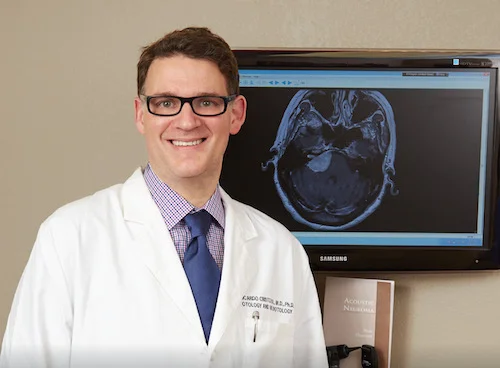
Acoustic Neuroma and Lateral Skull Base Disease
Acoustic Neuroma (Vestibular shwannoma)
What is an Acoustic Neuroma?
An Acoustic Neuroma is a benign growth of the nerve bundle that connects the inner ear to the brain. More specifically, it is a growth of the sheath of the vestibular nerve or the nerve of balance. These tumors are diagnosed in approximately 1 per 100,000 people per year. In most instances (95%) Acoustic Neuromas occur spontaneously with no attributable cause, although in a small percentage of patients, acoustic neuromas can be associated with Neurofibromatosis Type 2 (NF2), a hereditary genetic disease. The nerve of balance is intimately associated with the auditory and the facial nerves. As the tumor grows it affects the surrounding structures.
Attributed: UFHealth
Symptoms
The most common presenting symptom is asymmetrical hearing loss (reduction in hearing in one ear), imbalance/vertigo, and tinnitus or ringing in the affected side. Large tumors can have additional symptoms, such as facial numbness, headaches, and more rarely, difficulty swallowing with facial palsy or twitching.
Diagnostic tests
The most useful diagnostic test is magnetic resonance imaging (MRI) with contrast. This test allows detailed evaluation of the size, characteristics and location of the tumor. Such information is essential for selecting the most appropriate treatment modality. Hearing tests are also very important in deciding the management course. If medically indicated, further evaluation of the balance function of the ears can help select the best treatment modality. Many other factors are taken into consideration when deciding the form of treatment, including patient’s age, circumstances, preferences, symptoms, availability for long term follow-up and surgical and radiation therapy resources.
Treatment & Procedures
Acoustic neuromas can be treated with close monitoring, radiation or with surgery. In most cases small tumors (<1.5 cm) in asymptomatic patients can be followed with serial MRI imaging. In some patients, tumors may remain unchanged in size. It is important that the patients understand that the tumor remains intra-cranially and may go into a growth period at any time, thus repeat imaging over time is imperative. For medium (1.5 - 2.5 cm) and large tumors (>2.5cm), radiation or surgery is generally the necessary approach.
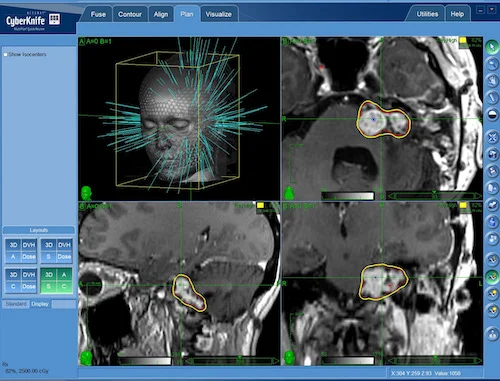
Stereotactic or three-dimensional radiation: This technology allows the delivery of a therapeutic radiation dose to the tumor while the surrounding tissue only receives a small safe dose of radiation. Different systems are available (Gamma Knife, Cyberknife, Novalis, etc).
Cyberknife
Surgical micro-dissection: This is oftentimes reserved for large tumors, symptomatic patients or very small tumors with intact hearing in healthy patients. Different skull base approaches are available to the surgeon and each has its have advantages and disadvantages. Dr. Cristobal will typically discuss these with you during your pre-operative appointment.
Translabyrinthine approach: With this approach the incision is made directly behind the affected ear. It is a safer approach regarding the facial nerve as it is visualized at the very beginning of the surgery. This advantage may prevent facial weakness or paralysis after the surgery. However a disadvantage to this approach is that it does not preserve residual hearing. Meaning there will be a complete loss of hearing on the operated side.
Suboccipital approach: With this approach the incision is made behind the ear, however somewhat farther back when compared to the Translabyrinthine approach. This approach oftentimes will ensure preservation of hearing when utilized for the removal of small tumors.
Middle Fossa approach: With this approach the incision is made in front of the ear. This approach will also ensure preservation of hearing. However it is reserved for small tumors within the internal auditory canal.
Learn more about Acoustic Neuromas by visiting the site below:
Paraganglioma (Glomus tumor)
Glomus tumors are a family of benign growths that originate in blood vessels. They are the most common tumor of the middle ear and second most common of the temporal bone. These tumors are very slow growing and initially present with vague symptoms of ear fullness, pain, and the sensation of hearing the pulse. Oftentimes, patients seek help when the tumor is fairly enlarged. If left untreated the tumor can cause hearing loss, tinnitus, facial weakness, loss of balance function, difficulty swallowing, hoarseness, and extend into the skull causing brain compression symptoms. They may be treated with monitoring with serial imaging studies, stereotactic or focused radiation or with surgical removal. Doctor Cristobal discusses with patients the advantages and issues with each treatment type and assists the patients in deciding the best plan for each one.
Meningioma
A meningioma is a form of tumor found arising in the meninges (the membranes that cover the spinal cord and brain inside of the skull). It is the most common type of tumor originating in the central nervous system. As many as 90% of these tumors are non-cancerous and often slow growing. The majority of people with a meningioma do not have symptoms and do not require treatment. However, a small number of meningiomas are found to be cancerous. These may grow rapidly and infrequently spread to other areas of the body. For this reason, any time a meningioma is discovered, it must be monitored closely with routine imaging studies and symptom assessments.
Symptoms are commonly related to the size of the tumor. Many people with a meningioma do not have symptoms because the majority are small and slow growing. If the tumor grows large enough, symptoms may gradually develop. The most common symptoms include headaches, blurred vision, numbness, weakness in arms or legs, speech problems, and seizures. Meningiomas are usually diagnosed when a patient is experiencing symptoms or are found incidentally with imaging of the head for other reasons. When meningiomas are large and/or growing rapidly, treatment with surgical removal and/or radiation is warranted.
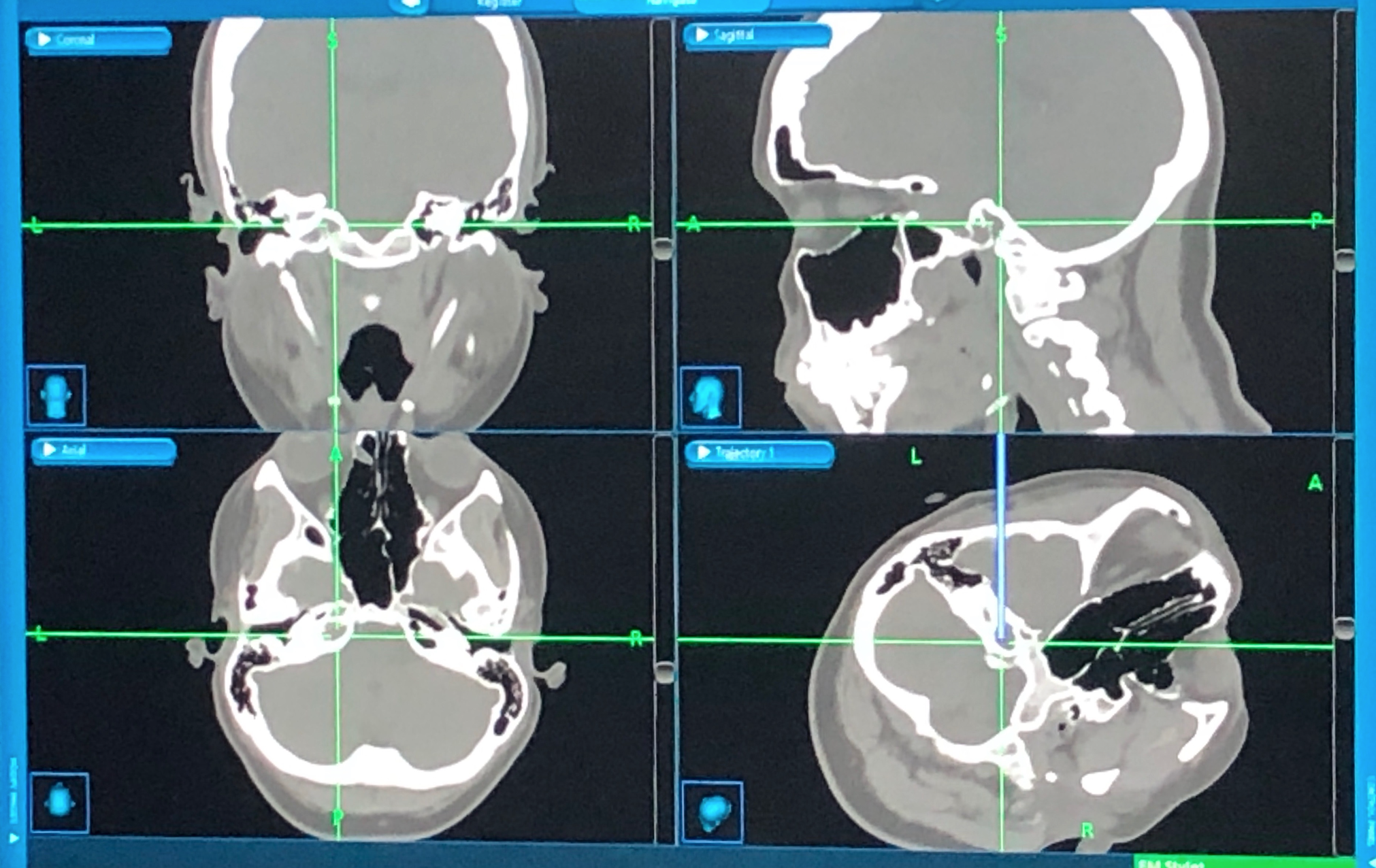
Cholesterol Granuloma of the petrous apex
Cholesterol Granulomas are uncommon cyst-like masses, which can form in any aerated portion of the temporal bone. These tumors are benign (non-cancerous), but can be dangerous depending on their location. When cholesterol granulomas occur in an area called the petrous apex, depending on their size, they can cause problems such as permanent hearing loss, bone destruction and damage to nearby nerves. Patients may experience headaches, pain behind the ear, hearing loss in one ear, vertigo, and ringing in the ears (tinnitus). Cranial nerve dysfunction can also occur, causing symptoms such as facial numbness, twitching, or weakness, and double vision.
Treatment interventions are based on presence of symptoms, ongoing growth and the size and location of the lesion. Observation by obtaining routine CT and/or MRIs of the head is an acceptable treatment option for those patients without symptoms or those in poor health and unable to undergo general anesthesia. Surgery is reserved for those patients who are symptomatic, become symptomatic after monitoring, or with lesions that are larger or have grown significantly.
Osteomyelitis of the skull base
Osteomyelitis is an infection of the bone. Osteomyelitis of the skull base is a relatively rare but serious medical condition. It is most commonly secondary to an infectious process such as inadequately treated and chronic infections of the ear canal. A history of diabetes, those who are immune-compromised, or those with micro vascular disease significantly are at increased risk for osteomyelitis. Suspicion for osteomyelitis of the bone around the ear and skull base should be raised in a patient with the previously discussed medical history and a persistent headache accompanied with cranial nerve deficits including hoarseness and difficulty swallowing. Treatment consists of long-term antibiotics for a period of 6 weeks with the consideration of hyperbaric oxygen therapy in the case of chronic, recurrent osteomyelitis. Surgical intervention is usually not indicated, however may be warranted if an abscess is present or in cases of poor response to intravenous antibiotics.
Cerebral spinal fluid (CSF) leak and TEMPORAL encephalocele
Cerebral spinal fluid (CSF) is a clear liquid that surrounds and protects the brain and spinal cord. A membrane called the dura surrounds the CSF to keep it in place. Any damage to the dura can result in the leakage of CSF. Damage can occur from head injury, spinal taps, epidural anesthesia placement, and certain head, brain, or spinal surgeries. Sometimes when patients suffer from chronic ear infections, the temporal bone can begin to erode away, causing an exposure of meninges or brain tissue, called an encephalocele. These patients can also develop CSF leakage into the space behind the eardrum (the middle ear space).
Common symptoms include chronic fluid accumulation behind the eardrum with fullness, pressure and hearing loss. Since the middle ear connects to the nose through the Eustachian tube, some patients may develop a steady dripping of clear fluid from the nose when leaning forward, or into the back of the throat. Patients also commonly experience a headache that improves when lying down and becomes more intense when sitting up or standing. To confirm the diagnosis of CSF leak, imaging such as CT head/temporal, CT cisternogram or MRI of the head are usually obtained. CSF can also be collected and sent for laboratory testing. Once confirmation of a CSF leak is made, surgical intervention is based on the site of injury.